- Medical Extruded Tubing
- Medical Reinforced Tubing
- Polyimide
- PEEK
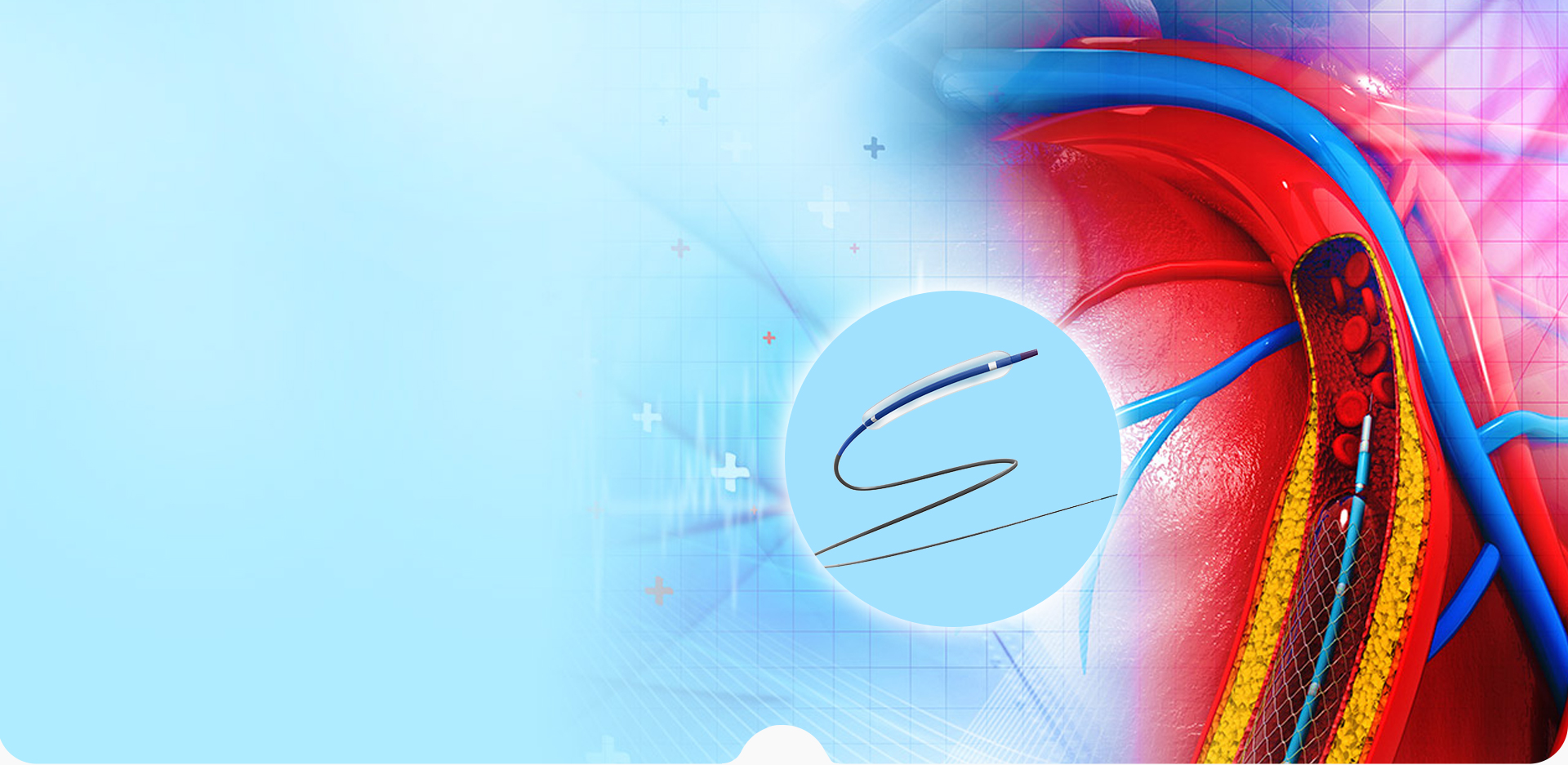
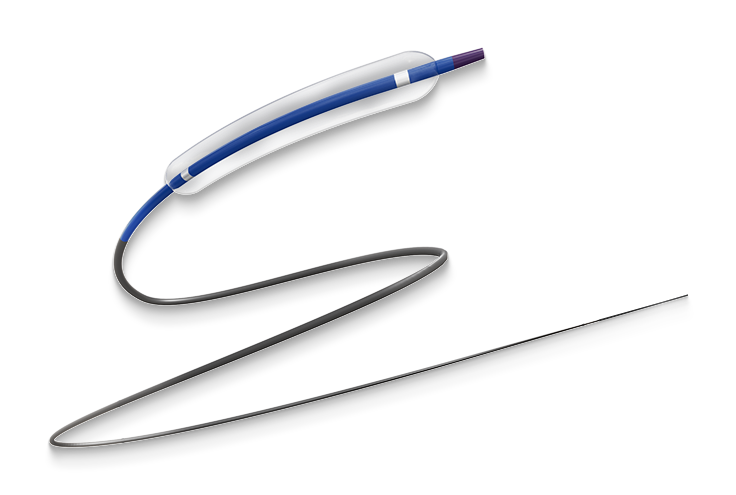
- Balloon Tubing
- Micro Catheter
- Secondary Processes
- Heat Shrink Tube
- Fluoropolymer Medical Tubing
- Endoscope
- Negative Pressure Access Sheath
- Guiding Catheter
- Angiographic Catheter
- High Pressure Braided Tubing
- Medical Tubing Surface Treatment Process
OUR PROVIDED
PRODUCTS
LINSTANT has always considered independent innovation as one of its core values. We can lead the enterprise and push the industry to a new stage through continuous self-driven research, development, and innovation.


-
CUSTOMIZED FORYOUR BUSINESSTailored for a Wide Range of Applications
-
Research and DesignWith an in-depth understanding of the properties of polymer materials and the application requirements of medical catheters, we leverage our extensive experience in R&D and design to offer constructive material selection and design recommendations tailored to your needs.READ MORE
-
Rapid PrototypingEquipped with a comprehensive production process system and advanced processing equipment, we adhere to design specifications to swiftly manufacture prototypes. We maintain frequent and in-depth communication with you to ensure that the appearance quality, dimensional accuracy, and basic performance indicators of the prototypes meet your design expectations. Additionally, our rapid prototyping line enables fast sampling, saving you time and costs.READ MORE
-
Testing & ValidationWe collaborate with your validation processes and provide the samples and documentation required for clinical trials and other regulatory needs. We also offer professional guidance on product and regulatory matters.READ MORE
-
Certification AssistanceWe are certified to ISO 13485 quality management system. Our robust quality management system provides comprehensive support to ensure that all documentation complies with regulatory requirements, facilitating a smooth product certification process.READ MORE
-
Mass ProductionWe have a mature production management system and strictly follow standardized processes to ensure timely, high-quality, and accurate delivery. In the event of quality issues, we immediately initiate a traceability mechanism to pinpoint the root cause and implement swift corrective actions, ensuring that every product entering the market meets stringent quality standards.READ MORE

INDUSTRIES
WE SERVE
We understand challenges in various industries and provide solutions to meet your specific production needs.
READ MORE
ABOUT
LINSTANT
Ningbo Linstant Polymer Materials Co., Ltd. was a professional
READ MORE
OEM/ODM Medical Tubing Manufacturers and Medical Tubing Supplier
, established in 2014 and now employs over 400 employees. We specialize in the extrusion processing, coating, and post-processing technologies of medical polymer tubing. Our commitment to medical device manufacturers is reflected in our precision, safety, diverse processing capabilities, and consistent product quality.-
0Establishment time
-
0+Employee
-
0+Production line



 English
English  Français
Français  Español
Español  简体中文
简体中文
 简体中文
简体中文